While one can easily agree that the state of well-being affects psycho-physical health and performance, obtaining a suitable picture for assessing overall well-being is far from easy. In order to promote health recovery, one has to evaluate all types of unbalances that, though not resulting in defined clinical outcomes, lead to a poorer quality of life. In terms of subjective perception of well-being, one could start with the onset of Medically Unexplained Symptoms (MUS), that is to say, a variety of sub-clinical functional disorders that have been broadly investigated in international literature:
This type of symptoms, though not qualifying specific diseases, are indicative of an impaired physiological balance of the body, often correlated to inflammatory processes becoming chronic, improper dietary habits, alterations of physiological hormonal balances or of their physiological circadian rhythm.
In order to improve psycho-physical health, it is necessary to fill the (often neglected) gap between state of well-being and state of disease, without assuming that health means absence of disease.
The onset of MUS is a non-negligible index related to metabolic or neuroendocrine disorders. An investigation into the causes of these symptoms, combined with specific recovery strategies, enables symptom mitigation and remission and prevents the factors involved in symptom origination from worsening and entailing additional and more severe systemic interactions that could result in specific diseases.
Still, MUS are non-specific: as such, they neither fit into a single group nor benefit from a single treatment, given that a symptom can originate from a variety of issues or from the concomitant interaction of pathogenetic processes of a different nature.
As a result, when dealing with a specified case, one has to compare and correlate multiple data above and beyond medically-unexplained symptoms.
Indexes of primary importance can be obtained through tests for the clinical analysis of body composition (BIA-ACC device), heart rate variability (HRV) and the Autonomic Nervous System (PPG Stress Flow device). No doubt, monitoring the level of hydration, intra- and extra-cellular fluid distribution, skeletal muscle, types of fat, quantity and quality of minerals and regulation capacity of the autonomic nervous system (Heart Rate Variability - HRV) play a crucial role in view of a complete evaluation of the state of health.
The analysis of body composition enables to monitor the fundamental parameters of skeletal muscle (FFM, Skeletal Muscle and SMI). In fact, the tendency to lose skeletal muscle is not a rare occurrence, regardless of whether it is linked to endocrine, metabolic or chronic inflammatory disorders. Therefore, before making any dietary changes or establishing precise recovery strategies, one should consider a periodical instrumental measurement of the ratio between Skeletal Muscle, Fat Mass (FM) and types of fat - intra-muscular fat (IMAT) and visceral fat (AAT).
Besides, in view of improving dietary habits, one should not underestimate the value of basal and daily metabolism (BMR, 24EE) as these parameters are closely related to the patient’s metabolic state and to the ratio between skeletal muscle and fat mass.
However, skeletal muscle preservation is not the only aspect that affects body metabolism, as the latter can suffer mild or substantial changes also as a result of chronic inflammation and the related level of systemic inflammation. As a matter of fact, persistent inflammation stimulates neuro-immunoendocrine alterations and hence entails a modification of metabolism – as a rule, decreasing a patient’s metabolic capacity. Clinical analysis of the body bio-impedance has been proven to be useful for this purpose to the extent that it can express the value of the HPA axis index (cortisol rhythm), that indicates the integrity of cell membranes and correlates to the level of systemic inflammation and to the loss of intracellular fluids and skeletal muscle.
In addition to systemic parameters, the overall state of health can be further clarified by an investigation into the regulation and adaptation capacity based on the analysis of the autonomic nervous system, which enables to evaluate the degree of endogenous anti-inflammatory regulation, highlighting the factors that play a role in symptom origination and loss of psycho-physical health.
BioTekna Plus is an integrated platform for an instrumental, nutritional, physical and motor assessment. It provides information on the level of extracellular acidosis (which can vary significantly whenever the homeostatic balance is altered and is therefore fundamental for recovery) and the possible the need for supplements, as calibrated based on specific data (Melcalin).
This general picture can be further enhanced by analyzing the function of the neuro-immunoendocrine system and hence the patient’s hormonal status, pointing out alterations of the function or daily rhythm of endocrine glands and of the related hormonal interactions. Excessive hormonal stress, in particular of the adrenals, often entails alterations in insulin response to food, which correlates with metabolic disorders or changes.
The BioTekna Plus software platform enables to relate all of the parameters mentioned above to dietary habits as it analyzes, and summarizes in the Health Radar chart, the parameters of the body composition, autonomic nervous system and heart rate variability tests, as well as the data captured from validated interviews on medically-unexplained symptoms and dietary habits: the overall processing of this information enables to evaluate the 24-hour metabolic response, i.e., glycemic load (GL), potential renal acid load (PRAL), final products of glycation AGEs) pointing out issues related to the response of the body to the daily intake of food.
The system described above integrates instrumental and lifestyle parameters; as such, it has a considerable potential in that it provides a complete picture that enables to detect a variety of conditions, be they systemic or local. An additional benefit is real-time simulation of the behavior of specific dietary corrections of nutrition status, which enables to identify precise physical and nutritional strategies aimed to restore well-being, with the additional indication of the possible need for supplements in the event of nutrients deficiency (buffer systems, antioxidants, etc.).
A synergistic application of all interventions improves overall well-being, i.e., hormonal state regulation, increased metabolism and skeletal muscle, increased hydration and decreased systemic chronic inflammation - all of which have a direct connection with MUS. The immediate perception of improvement, thanks to the disappearance of MUS, is confirmed by the patient’s improved quality of life, which is often forgotten in the programs for the recovery of psycho-physical wellness.
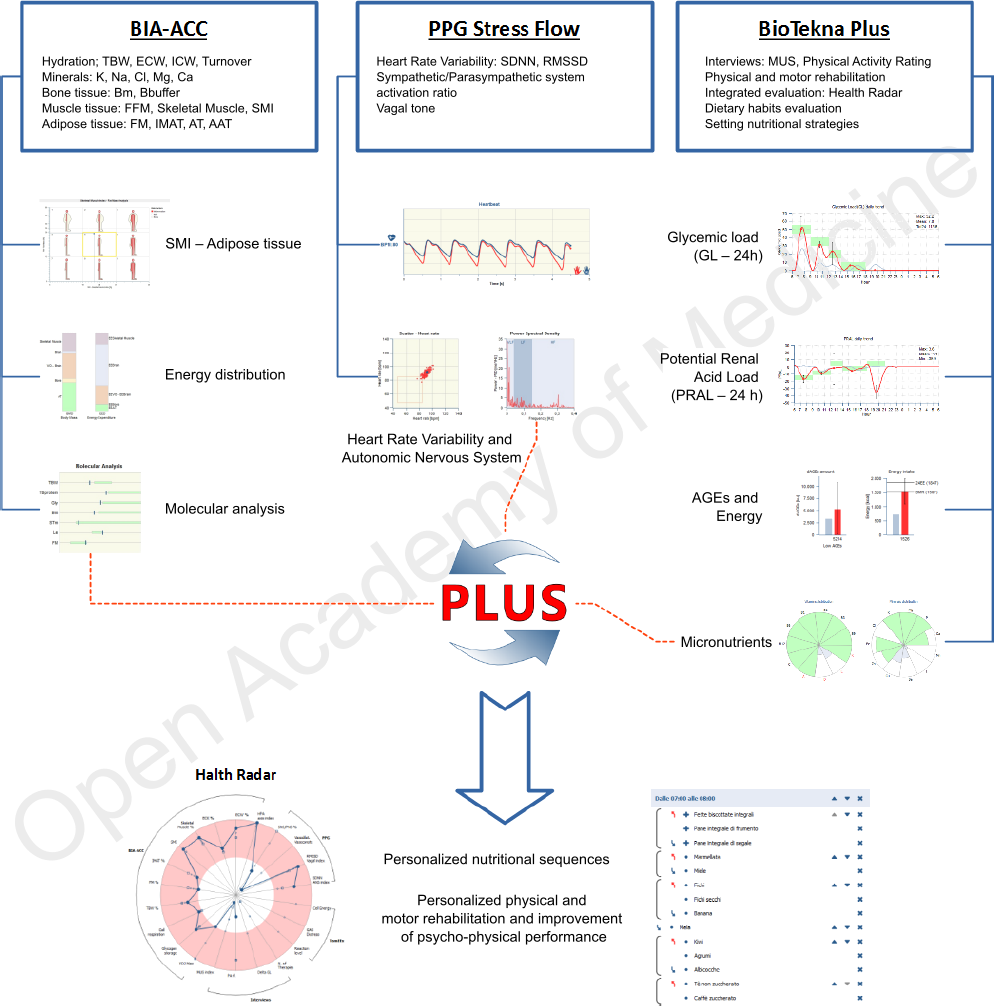
Figure 1: Integrated evaluation of Body Composition and Heart Rate Variability
Author: Dario Boschiero - Date: 27/03/2019
Attention: these contents can be freely used for personal learning purposes only. The use is regulated by Law No. 633/1941 and subsequent amendments, as well as by the copyright and patent legislation in force. Any use for commercial and profit-making purposes is forbidden.