Changes in body composition respond, more or less rapidly, to what we eat and the exercise we do but not only to this. Loss of skeletal muscle (S-Score, Skeletal Muscle - BIA-ACC), increase in ectopic adipose tissue (IMAT - BIA-ACC), increase in Medically Unexplained Symptoms (MUS) and repeated clinical signs that in most cases result in a disease, are among the main causes of a worsening quality of life. [1-4]
Unfortunately, alongside these causes, many factors can but affect our skeletal muscle and hence our health. [5]
Physical inactivity is the single major cause of skeletal muscle loss, followed by malnutrition (arising from increased energy requirement, above all in case of severe diseases, over- or under-eating), dehydration, malabsorption and higher levels of proinflammatory cytokines (with increased production of reactive C protein, CRP). [6-9]
This broad range also includes long-term drug therapies. In fact, several classes of drugs cause a depletion of important mineral salts and vitamins that are indispensable for healthy skeletal muscle (e.g.: co-enzyme Q10 depletion due to long-term hypolipemic drug therapies, vitamin B12 depletion due to hypoglycemic drug therapies, etc.). In addition, as the liver metabolizes most drugs, long-term use of drugs impairs the production of albumin (produced by the liver and then released into the bloodstream).
Albumin is well worth a deep-dive into.
Indeed, albumin is the most abundant protein in our body, accounting for approximately 55% of total protein content. It is the main substance responsible for maintaining plasma oncotic pressure (as it is also the single, most abundant protein in plasma), regulates and modulates the distribution of fluids between intra- and extra-cellular compartments (ICW/ECW - BIA-ACC). [10,11]
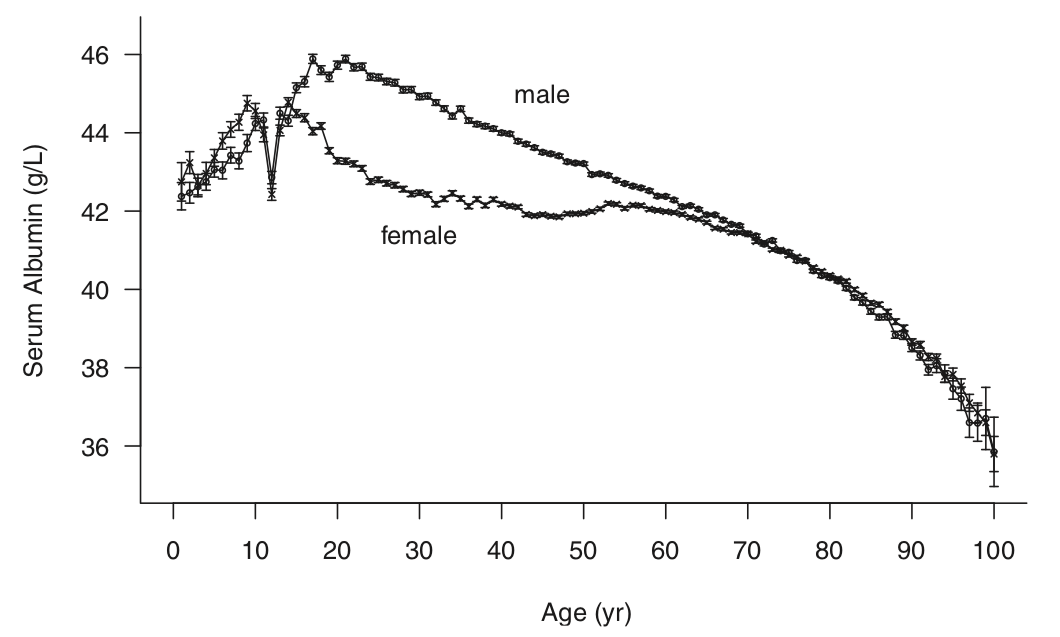
Figure 1: albumin serum concentration by gender and age [13].
Serum albumin is also used in clinical settings as a biomarker of malnutrition, cachexia and significant loss of skeletal muscle. [12]
In all cases of increased albumin requirement, albumin (egg protein) supplements with negative renal acid load buffer systems (PRAL -36) could play a role thanks to the benefits from the above-described properties of albumin added to those from negative PRAL (anti-inflammatory) diet.
Albumin supplements can therefore be advisable for skeletal muscle recovery, to help regulate acid-base balance, as a support due to their chelating activity (albumin is capable of binding to - and transporting - a broad variety of endogenous and exogenous substances, while performing a protective activity through the sequestration of toxic substances), or for those individuals who, because of a disease or their diet, are unable to take the proper amount of proteins to ensure a positive nitrogenous balance.
As to when to take albumin supplements, this varies depending on what one is aiming for:
- After workout, for recovery, considering their high biological power (100%) and lactate load lowering capacity (resulting from their negative acid load);
- Before dinner or before breakfast to help and support acid-base balance regulation and in case of malnourishment.
Authors: Dario Boschiero, Mariantonietta Lucafò - Date: 01/03/2021
Attention: these contents can be freely used for personal learning purposes only. The use is regulated by Law No. 633/1941 and subsequent amendments, as well as by the copyright and patent legislation in force. Any use for commercial and profit-making purposes is forbidden.
References