As a rule, hot and humid seasons record increasing cases of malaise and disorders linked to altered hydro-electrolytic balance. All population groups are at risk – more so in recent years due to worsening climate change.
As a result, a significantly higher amount of fluids is transferred to the outside environment (with body weight fluctuations up to kilograms in a single day). Besides being sizeable, these changes develop very fast, which often limits the ability to mitigate their consequences due to the disproportion between the amount of water and micro-elements lost by the body and their daily intake.
In this regard, one of the first issues that physicians or nutritionists are called upon to consider is an evaluation of the patient’s general state of hydration.
Having regard to this, our method of choice in outpatient settings is BIA-ACC (Bioelectrical Impedance Analyzer – Body Composition Analysis) as it is able to evaluate with a good level of precision a number of fundamental parameters relating to fluids distribution and body tissues (table 1).
Table 1: parameters that can be measured with the BIA-ACC test
In family practice and clinical nutrition, the BIA-ACC test is not used to monitor daily changes in the level of hydration; rather, it is mostly used to estimate a patient’s systemic hydration so as to evaluate his/her exposure to the risk of dehydration.
Practice shows that the general level of hydration (TBW, Total Body Water) of most patients falls significantly short of the ideal level (i.e., 60% of the body weight). Clearly, the lower this parameter, the more prone the patient is to dehydration.
The loss of body water (TBW, Total Body Water) entails higher risks for the elderly, who are less able to balance of this loss, to the detriment of intra-cellular water (ICW, IntraCellular Water). Besides, dehydration occurs in parallel with the loss of electrolytes, thus further worsening the overall situation.
Preservation of the lean mass (FFM, Fat Free Mass) is key as this compartment is the hardest hit by dehydration, which comes as no surprise since most intra-cellular fluids are stored in muscle, organ and (though to a lesser extent) skeletal tissues.
Therefore, in a very hot environment, the elderly are more at risk for dehydration. Likewise, children, being more physically active, not infrequently run the same risk. So, one should stay focused on this risk, regardless of the age group considered.
A variety of factors, ranging from a general lack of thirst to the need to get used to drinking more, play a role, such that, in general, the large amount of water and electrolytes lost during the day is not restored.
Multiple experiences carried out in particularly unfavorable contexts (in sports medicine or high-thermal-stress work environments) show that the intake of solutions containing electrolytes, vitamins and carbohydrates counters the risk of dehydration more effectively than plain water.
Focusing on the level of body hydration is undoubtedly fundamental when needing to intervene on a patient’s state of wellbeing and becomes vital for more fragile patients, such as those described above. Indeed, as said earlier, the changes discussed here are particularly insidious in terms of both their magnitude and pace. Before considering long-term effects, such as the onset of medically-unexplained symptoms (MUS, Medically Unexplained Symptoms), it is therefore fundamental to monitor the states of “acute” dehydration, which can lead to multiple failures (heart, respiratory, kidney, etc.) and which are, in general, a non-negligible risk for patients’ safety.
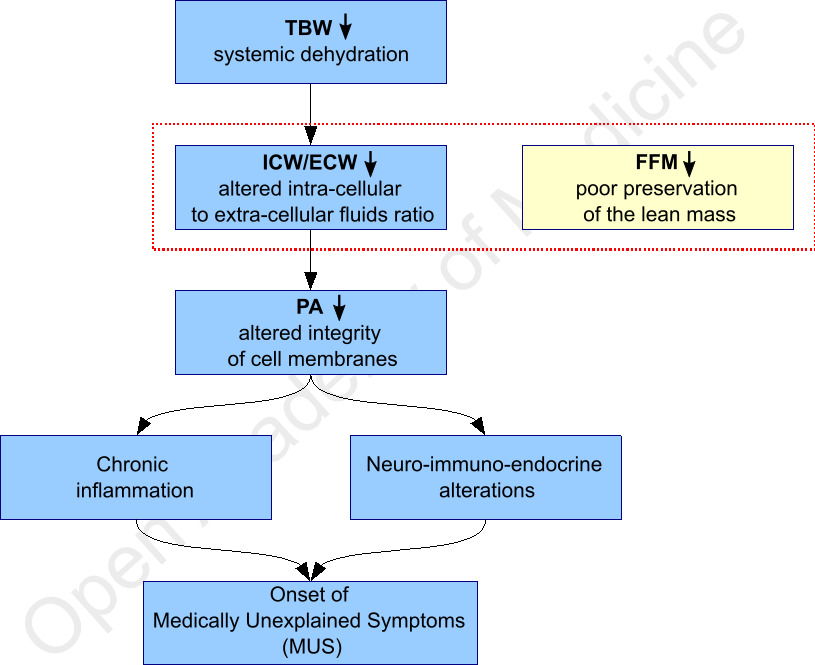
Figure 1: interactions between states of dehydration and onset of symptoms
The risk of dehydration is higher in patients with chronic disorders (of any description) as compared to those with acute conditions. This requires more focus on all patients with medically-unexplained symptoms (MUS, Medically Unexplained Symptoms, table 2), considering that, in many instances, these symptoms are ascribable to chronic inflammatory processes.
Table 2: Medically-Unexplained Symptoms (All Rights Reserved BioTekna – Italy. MUS® n.2012001626, 2012)
A variety of factors affect the efficacy of supplements for restoring the hydro-electrolytic balance: from the need for an ideal balance of micronutrients, minerals and vitamins, to the final aroma of the product. In fact, as observed many a times in clinical research, a drink’s flavor is not an element of lesser importance in view of making it more palatable than water, thus encouraging its consumption and limiting untoward effects (e.g. nausea) linked to consumption of large amounts of natural water. In addition, considering the same volume of water consumed, a solution that provides a proper supplementation of microelements provides greater protection from the loss of lean mass (FFM, Fat Free Mass) and intra-cellular body fluids (ICW, IntraCellular Water) due to heat. Among available options, an alkalinizing solution (containing, for example, bicarbonate-based buffer solutions) is no doubt advisable to promote proper acid-base balance, especially in patients with chronic inflammatory and acidosis.
Authors: Dario Boschiero, Alberto Semenzato - Date: 25/05/2007
Attention: these contents can be freely used for personal learning purposes only. The use is regulated by Law No. 633/1941 and subsequent amendments, as well as by the copyright and patent legislation in force. Any use for commercial and profit-making purposes is forbidden.
Further references