Albumin is an important protein for body homeostasis. It is produced by the liver and then released into the bloodstream. It is also present in egg albumen, after which it is named. Blood albumin concentration typically ranges from 3.5 to 5.0 g/dL and accounts for approximately 60% of all plasma proteins.
Albumin is the single most abundant protein in the human body as it accounts for at least 55% of total protein content.
Albumin is essential to regulate and maintain oncotic pressure, i.e. the osmotic pressure that is required for proper distribution of intra- and extra-cellular body fluids (ICW - ECW BIA-ACC body composition).
As albumin molecules are negatively charged, like the glomerular membrane of the kidney, electrostatic repulsion normally prevents albumin from passing into the urine.
In urinary tract and kidney diseases, diabetes and a variety of chronic inflammation, including low-grade inflammation conditions, this property is lost and, as a result, albumin is found in the urines.
For this reason, albumin is considered to be an important marker of disfunctions that may appear years later.
Every molecule of albumin has a half-life of 27 days and during this period of time it passes approximately 15,000 times in the bloodstream to carry out its functions, i.e.:
While albumin is synthesized by the liver, its production is regulated by a number of cytokines such as pro-inflammatory cytokines IL6 and TNF-α that induce downregulation.
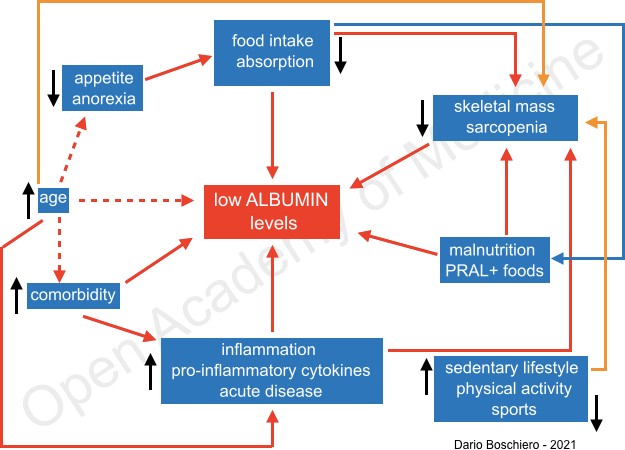
Figure 2: factors that lead to lower levels of Albumin (D. Boschiero)
Functions of albumin
Albumin and clinical correlations
Albumin and prognosis
A meta-analysis of 110 studies has found that albumin deficiency in patients indicates a poor prognosis of disorders and diseases.
Albumin as a marker
Albumin is a good marker of rapid changes in physical and nutritional status, reflects Sarcopenia, Cachexia, significant losses of fat-free mass (FFM) and in particular of skeletal muscle (S-Score BIA-ACC), malabsorption and loss of the minimum percentage of total proteins (TBprotein BIA-ACC).
PRALBUMIN: negative-charge buffered albumin
Purpose of supplementation:
Author: Dario Boschiero - Date: 17/09/2021
Attention: these contents can be freely used for personal learning purposes only. The use is regulated by Law No. 633/1941 and subsequent amendments, as well as by the copyright and patent legislation in force. Any use for commercial and profit-making purposes is forbidden.
References